Sept. 4, 2019
The sun came up again today. I saw it.
So many of the patients who came to Denise McClellan, Jason Pedwaydon and other personal trainers shared that sentiment in some way. Tomorrow wasn’t promised, but they had today. So they were going to make today count.
But they were going to do their best to make good on tomorrow, too.
That was the motivation for 82 participants in a study that looked at how physical activity helped Native American cancer survivors to heal, recover and find a healthy lifestyle. The study, which was part of the Partnership for Native American Cancer Prevention (NACP), was a collaborative effort between Northern Arizona University and the University of Arizona Cancer Center. Researchers looked at whether a program that included weekly exercise sessions with a trainer, combined with a home exercise program and regular health monitoring, could help the group become healthier.
The project ended Aug. 31, so it’s too soon to officially say yes, it does, but anecdotally—yes, it did.
“What we’re finding is just movement itself is rehabilitative,” said Brenda Charley, coordinator of the project. “That’s one reason we let friends and family in. We want to make sure they understand they’re doing something good for themselves too.”
The project focused on Navajo cancer survivors and their caregivers and Native American, mostly Navajo personal trainers—getting them valuable experience and preparing for certification to send them back to their communities with the skills needed to continue in this work.
The need for this research

For a long time, medical research tended to treat everyone as a monolith, not taking race, gender and other demographic factors into account. As a result, Native Americans’ unique needs were overlooked. Dirk de Heer, an associate professor of health sciences and principal investigator in the NACP, looked for holistic ways to fill that research gap that not only focused on Native Americans’ health but also met the research subjects where they were, leaving space for tradition as they worked out and tracked calories. If that meant wearing a Fitbit with ceremonial dress, then that’s what they did.
“There is an enormous need for translational research with the Navajo Nation and other tribal nations in our region,” de Heer said. “People often travel very far to receive care and screening, not to mention the additional barriers related to poverty and cultural misalignment in our health care system. Even more importantly, there is a need to train local personnel, support workforce development and work directly with regional providers.”
This gap is largely what the NACP was created to address; all of the associated researchers are asking cancer questions about Native populations. In 2013, the program sent out a call for pilot proposals on which NAU and U of A researchers collaborated. De Heer received recommendations from now-provost Diane Stearns, who was the NACP research lead at the time, and connected with NAU nursing professor Anna Schwartz and Jennifer Bea, a cancer exercise and body composition researcher at U of A. Etta Yazzie, an oncology nurse Arizona Oncology Associates, also joined the team as one of the few oncology providers in the region with in-depth knowledge of the Native American culture. Jointly, they developed a project aimed at Native American cancer survivors and how physical activity could help them live longer, healthier lives.
After the first round of research, they received funding for a five-year project and took on more partners, including the Native Americans for Community Action (NACA), the Leupp Chapter, research specialist Taylor Lane, now a Ph.D. student in interdisciplinary health at NAU, and several Native American students from both NAU and U of A, including Gold Axe winner Shelby Dalgai, Agassiz Writing Award winner Kaitlyn Haskie, former Miss Indigenous NAU Jayme Biakeddy and many others.
The focus group phase aimed at understanding barriers and facilitators to physical activity among cancer survivors. It was followed by a pilot study where the researchers developed and tested a physical activity intervention for cancer survivors. It started in Flagstaff and Leupp, but the researchers realized quickly that traveling further reduced clients’ likelihood of success, so they opened clinics in Tuba City and Winslow as well. They also realized Native Americans, who place a high value on family and community support, did better with access to that support, so the team expanded the study to include caregivers.
“This is incredibly important in the Native American culture and history of kinship,” de Heer said. “In addition, family members of cancer survivors are often themselves at higher risk of developing cancer, which makes a physical activity program an important preventive measure.”
The results bore out that early observation, he said; patients who participated with family members had increased motivation and adherence to the protocol as well as an easier time with logistics like getting to the training center.
Each participant signed up for an 18-week period. For 12 weeks, they would meet once a week with a trainer, talk about their progress, set goals, work through challenges and then get an exercise regimen for the next week. That regimen usually consisted of a certain number of minutes of cardio and several strength-training exercises that used body weight or resistance bands or pulled “weights” from the average person’s home, like soup can rows.
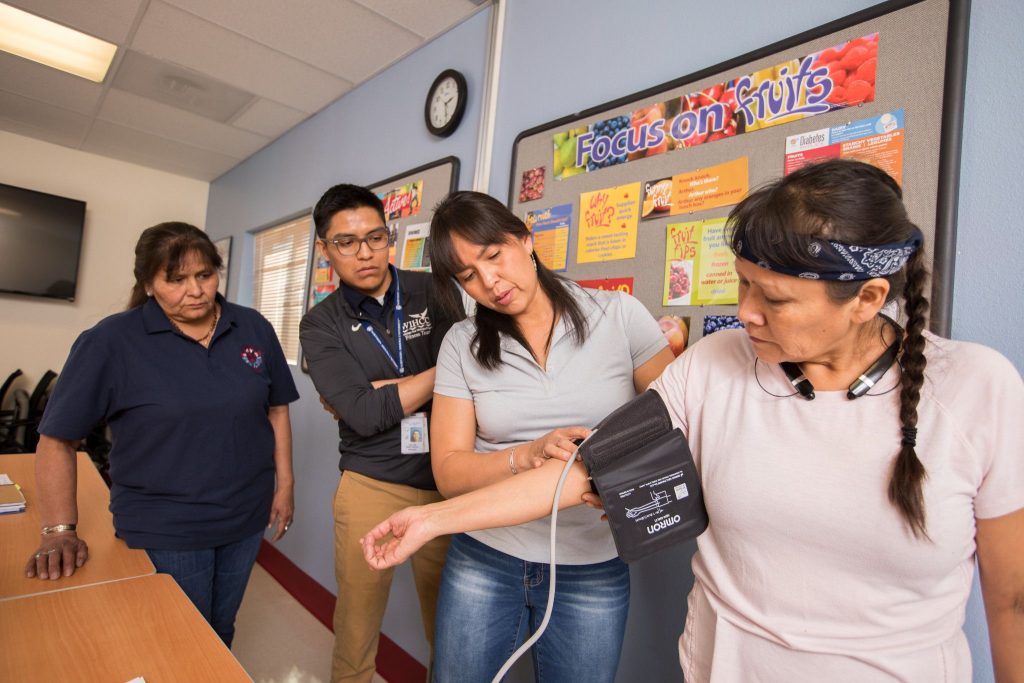
The participants also had a six-week period, either before they started the weekly sessions or after, where they were still providing data but not actively meeting with a trainer. Each participant had measurements, including weight, waist and hip size, A1C blood tests, blood pressure and other indicators taken at the start of the project and at six weeks, 12 weeks and 18 weeks.
The trainers also explained what those data meant, Charley said; often, patients didn’t know what an A1C reading was and whether their number was good or worrisome. (It’s a test that measures blood sugar and is used to diagnose Type 2 diabetes and prediabetes.)
It wasn’t always easy; Charley said technological issues like Fitbits simply not working on the reservation required the team to shift methodology as they went, resorting to questionnaires to gather information about food intake and how many minutes worked. And even the questionnaires weren’t all that effective; she found that most of the participants wrote little information down, but they were happy to sit down with her or a trainer and talk about what they’d done that week.
Although the trainers worked directly with clients, they had a conference call once a week with de Heer, Yazzie, Bea, Schwartz, Lane and Charley, discussing each client in-depth. The trainer working with each individual would explain that person’s progress and challenges, the regimen they’d just finished and the upcoming regimen they were considering. The experts would weigh in, making tweaks and providing direction as needed.
Finding Native solutions
Much of the motivation behind this study was to examine the beliefs and knowledge of Native Americans related to cancer, physical activity and treatment and then to turn around and use that knowledge to provide treatment that was in keeping with Native culture while also offering the best medical care possible.
A major component of this is the personal trainers themselves, who coached participants through exercises, talked to them about how they were feeling and explained how they might not have lost weight, but they lost inches and gained skeletal muscle and that’s even better. Because all of the trainers were Native, they understood the traditions and the prayers and the directions from a medicine man. When a client came in having just done a ceremony, wearing ceremonial clothing and unable to do certain tasks, the trainers took it in stride and worked around those limitations. Once, McClellan conducted client sessions in ceremonial dress. No explanation was needed.
“We had to be creative in not letting them feel uncomfortable because they came dressed the way they were, with those kinds of limitations,” Charley said.
The mutual understanding of tribal traditions and belief made these training gyms a safe place for clients. Although it’s too soon to know the data, anecdotally, the trainers said they saw differences. They saw commitment and desire and understanding.
“Many of them haven’t exercised because they don’t know what good exercise feels like, what movement can do for them mentally, physically and emotionally,” Charley said. “Or they forgot. A lot of them talk about their childhood, how they used to run all the time and be out playing, then they grew up and forgot how to do those things. Our job is to connect them back to it.”

The trainers are more than happy to be that link. Pedwaydon, who is of the Ottawa, Chippewa and Delaware tribes, is a cancer survivor. He talks about how his uncle, a medicine man, told him not to pound the earth or he risked the cancer returning. Pedwaydon put his snowboard away forever.
“Cancer sucks,” he said, to nods from his fellow trainers. “To see these individuals who are patients—survivors—trying to help themselves, and this is a new concept for them, that exercise is medicine. And guess what? You need medicine.”
One memorable day western and Native medicine collided for Pedwaydon. One of his clients showed up with a small bag. They walked through the PT routine, and the man kept the bag close, shifting it around as he performed the exercises.
Finally, Pedwaydon asked him what was in the bag.
“That’s my medicine,” the client said matter-of-factly. “It’s my chemo.”
For McClellan, who is Navajo, the difference is more than physical. She watched patients watch out with greater confidence in themselves and their ability to heal and become stronger.
“They start to live it, is what they do,” she said. “We assign their at-home programs, and they try to implement it in their lives. And most of them did! They applied it in their lives.”
“That’s where you guys come in,” said Anthony Santos with a nod. Santos, a second-year Ph.D. student in the interdisciplinary health program, oversees the trainers, including helping them study for the ACSM certification. “You can travel all over the Navajo Nation and can confidently educate and push people toward a healthier lifestyle. You can be a true service to the Navajo people for sure.”
That’s also what de Heer and his collaborators envisioned when the program started. It’s why they—a team of certified, highly qualified health professionals—are not on the ground working with clinics. Preparing the trainers for continued work with Native people after the study has ended is a critical outcome.
“Local trainers and workforce development are incredibly important for sustainability of everything we try to do,” de Heer said. “They live in the communities we work in, and supporting their career development is as important as our intervention. The knowledge and experience they build will carry on and continue to help their communities.”

Results and next steps
At this point, they’re preliminary, but the data show positive trends in weight loss at six weeks and fitness and quality of life at 12 weeks. Plus, patients just reported feeling better, with more energy and more excitement for life.
The team will continue studying the data, looking at possible next steps in approaching Native Americans’ approach to cancer care. The findings for this study will be presented at the Navajo Human Research Review Board Conference in October and the American Association for Cancer Research on Cancer Health Disparities in September.
Besides the benefits to cancer research, students who participated in this program also saw benefits. Many Native American students have gone on to medical school, graduate programs in public health and completed internships and fellowships at organizations like the National Institutes of Health and Harvard. De Heer said, in addition to the NACP (which is funded in part by the NIH), donations from the John and Sophie Ottens Foundation made such internships possible.
“It is my hope that these students will not only support but lead many projects in their own communities in the future that address the needs of cancer survivors and their families,” de Heer said.

Heidi Toth | NAU Communications
(928) 523-8737 | heidi.toth@nau.edu



