Collaborative research between the three major Arizona universities is helping young people with cerebral palsy (CP) to walk more confidently and safely on their own.
This research, led by Northern Arizona University mechanical engineering assistant professor Zach Lerner, uses wearable robotic devices to assist a person’s gait and to provide tools that help to retrain their legs how to walk. Lerner, who holds a dual research appointment at the University of Arizona College of Medicine-Phoenix, is working with colleagues from UArizona and Arizona State University at the Phoenix Biomedical Center (PBC).
The study, published in the IEEE Open Journal of Engineering in Medicine and Biology, looked at six children with cerebral palsy. Each child came in to the PBC for 10 training sessions with this device; the goal was to measure and retrain each child’s walking gait by strengthening plantar flexors, increasing their speed and reducing the amount of energy needed to walk.
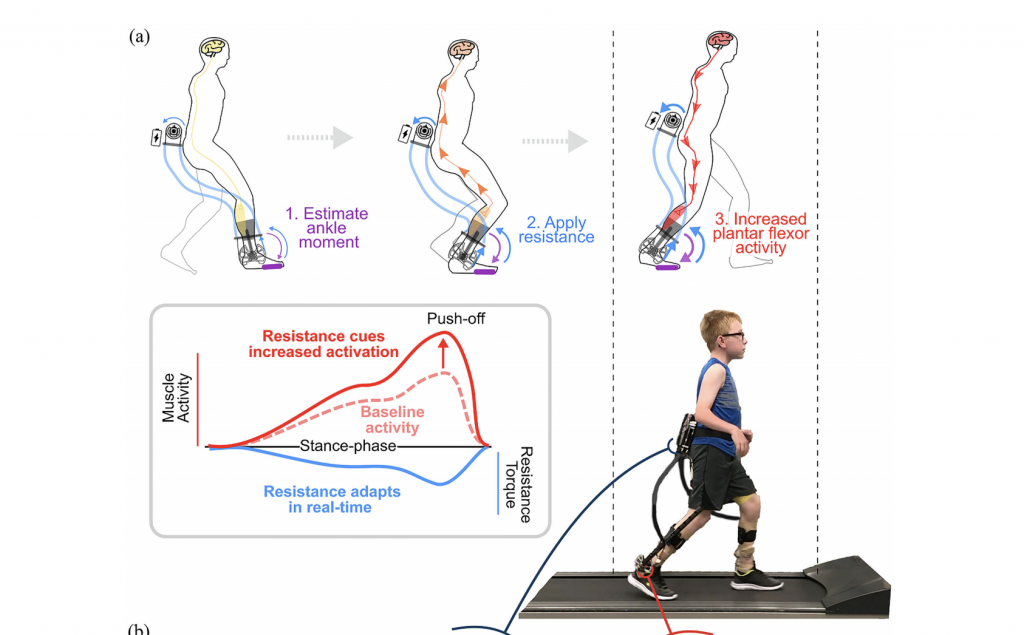
The wearable device, which added targeted resistance depending on how the child was walking, also provided immediate feedback so the researchers could determine how well the child was doing and what needed to be adjusted, which contributed to better outcomes for every child who participated in the study.
“Most exoskeleton research has been conducted to provide assistance, aimed at making walking easier. We did the opposite. We used an exoskeleton to provide targeted resistance for neuromuscular gait retraining, aimed at improving long-term function,” Lerner said. “We also used immediate sensorimotor feedback, which we think is really critical for training the participants to use their own muscles more efficiently.”
Although the study size was small and lacked a control group, Lerner is pleased with the results of the study, which showed that wearable adaptive resistance training was a feasible and effective tool in improving mobility for individuals with CP, even those with ingrained walking patterns who needed to be retrained. With four weeks of training, every participant improved in every measure of success.
“We expect that this intervention may be suitable for other patient populations affected by neuromuscular impairment because it aligns with the guiding principles of neuroplasticity—task specificity and top-down active engagement,” the study reads. “This relatively low-cost, battery-powered and wearable intervention was designed for translation to both clinical practice and personal use at home, and as an untethered device, training can take place under a variety of contexts, including overground walking. The inherent accessibility of this wearable intervention provides individuals with the opportunity to significantly increase the frequency of targeted neuromuscular rehabilitation.
The likely next step for this research is completing additional exoskeleton gait rehabilitation studies at PBC, which is helpful for recruiting larger and more diverse participants.