Antibiotic-resistant infections should be easier to detect, and hospitals could become safer, thanks to a technology developed by the Translational Genomics Research Institute and Northern Arizona University, and protected under a patent issued by Australia.
Soon, similar patent approvals are expected by the United States, Canada, European Union, Japan, Brazil and other nations for this superbug test developed by TGen and NAU, and licensed to DxNA LLC, a company based in St. George, Utah.
“This rapid, one-hour test will precisely identify a family of antibiotic-resistant staph infections we broadly refer to as MRSA,” said Paul Keim, director of TGen’s Pathogen Genomics Division, or TGen North, based in Flagstaff.
“We hope this technology will be adopted worldwide by hospitals and clinics, and will help identify and isolate these dangerous and difficult-to-eliminate infections that have come to plague our medical institutions,” said Keim, who also is the Cowden Endowed Chair of Microbiology at NAU, and director of NAU’s Center for Microbial Genetics and Genomics. “The result should be more rapid diagnosis, improved treatment of patients and reduced medical costs.”
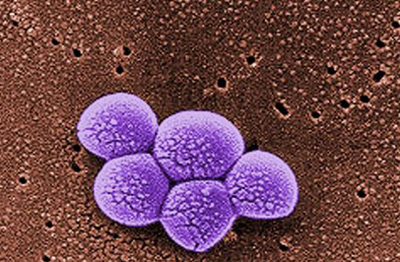
MRSA—methicillin-resistant Staphylococcus aureus—is an antibiotic-resistant form of the staph bacteria that annually kills more Americans than HIV.
While MRSA technically refers to one particular strain of staph, the genomics-based test developed by TGen, NAU and DxNA can precisely detect multiple types of drug-resistant staph bacterial infections, including drug resistant Coagulase Negative Staphylococcus, a much more common infection than MRSA.
Staph infections are the most common hospital-acquired or associated infections. While most of the focus over the past few years has been on MRSA, in terms of incidence and total cost, strains of staph other than MRSA are a much more common problem.
Due to the increasing use of implantable biomaterials and medical devices, infections are increasingly caused by Coagulase Negative Staphylococcus. This is a type of staph that is often resistant to multiple antibiotics and has a particular affinity for these devices.
“Rapid identification and differentiation of these resistant bacteria is key to optimizing treatment decisions that significantly impact patient outcomes and cost of care,” said David Taus, CEO of DxNA LLC. “Given that resistant CNS is a frequent pathogen in surgical site infections, orthopedic and cardiac device infections, and blood stream infections—among others—it is critical that we be able to rapidly identify and determine antibiotic resistance to provide for appropriate pre-surgical antibiotic prophylaxis to prevent infections and early and effective treatment when these infections do occur.”
Current molecular tests for MRSA all ignore CNS, rendering their results less useful in treating patients given that drug resistant CNS infections are many times more common than MRSA.
DxNA’s Staphylococcus test identifies and differentiates resistant and non-resistant strains of staph and CNS. The test uses three separate proprietary biomarker targets and a proprietary methodology to determine which types of staph are present, and which carry the gene that causes antibiotic-resistance in these bacteria.
“The test also is effective in identifying infected specimens where there are multiple types of staph. The test will rapidly provide broader clinically actionable results, improving early intervention and resulting in more effective treatment at lower costs,” Taus said.